Management of NSCLC
Work up
- Blood tests
- PFT
- Biopsy
- Molecular markers
- PET CT
- MRI Brain
- EBUS
Treatment Modalities
- Surgery
- Open vs. VATS or Robotic-assisted Approaches
- Lobectomy vs. Pneumonectomy vs. Sublobar Resection
- Systemic Therapy
- Chemotherapy
- Targeted Therapy
- Immunotherapy
- Radiation
- External Beam Radiation Therapy
- 3-Dimensional Conformal Radiation Therapy (3-D CRT)
- Intensity Modulated Radiation Therapy (IMRT)
- Stereotactic Body Radiation Therapy (SBRT/SABR)
- Proton Therapy (PT)
- External Beam Radiation Therapy
Basic Principles of Surgical Selection
- The definition of medically inoperable varies substantially between surgeons
- PFTs that suggest a patient should tolerate surgery include:
- Pre-op FEV1 >1.8-2 L (or ≥80% predicted) if patient needs a pneumonectomy
- Pre-op FEV1 >1.2-1.5L if patient needs a lobectomy
- Predicted post-op FEV1 >800 mL (>40% predicted)
- DLCO > 50-60%
- Resection of tumor in a dominant area of emphysema may have less impact on post-op lung function
- Patients with cardiac risk factors should have a preoperative cardiologic evaluation
- Contemporary 30-day mortality rates are 1-3% for lobectomy or sublobar resection and 2-11% for pneumonectomy
Active smokers have a mildly increased risk of post-op complications
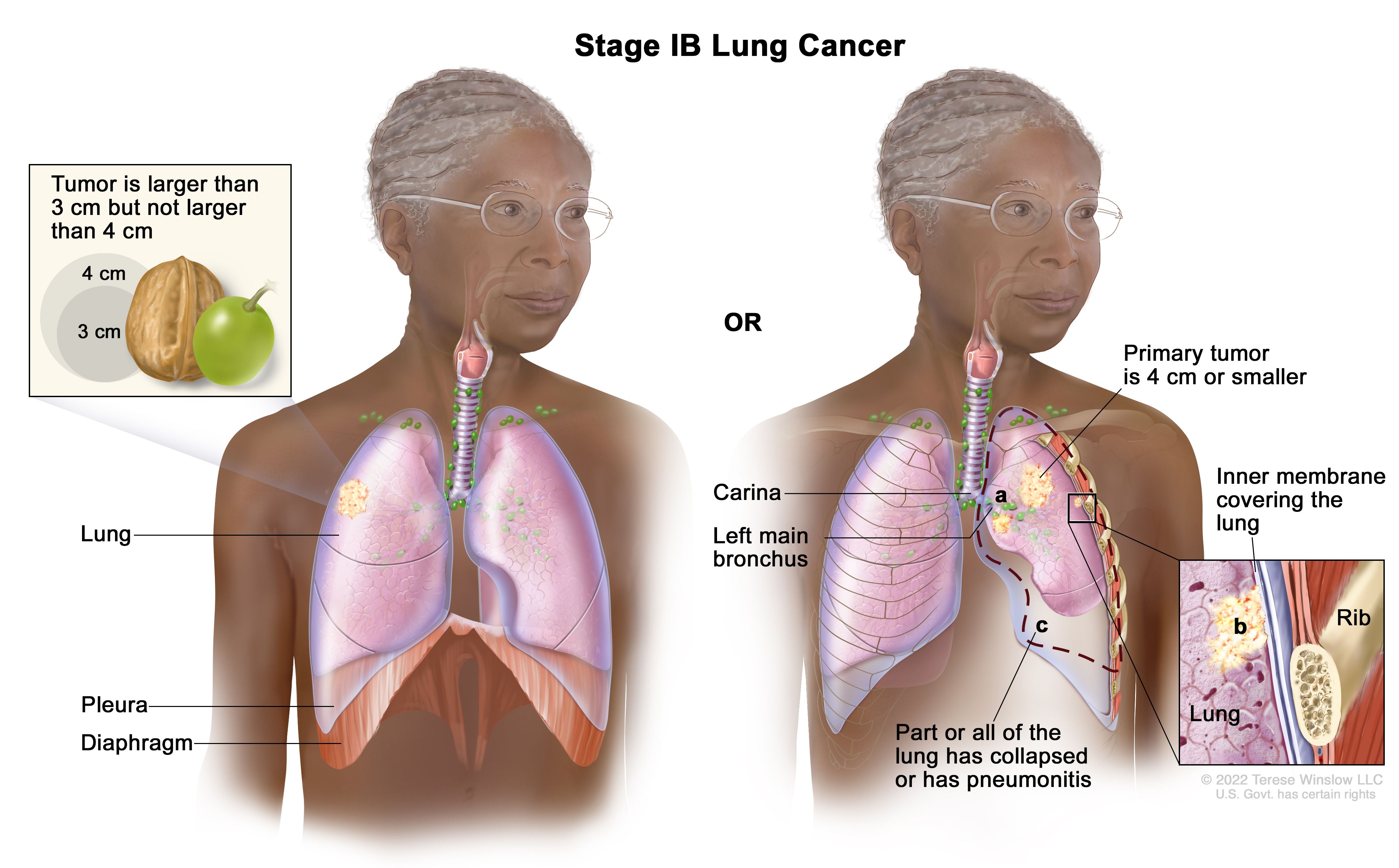
Management of Stage I + II NSCLC
-Surgery alone is the standard treatment choice !
-Lobectomy: optimal procedure
-Wedge resection: 3x LR/ 30% more mortality (Ginsberg 1995) but newer series show no worse outcome with limited surgery (Lee 2003, El Sherif 2006)
-Wedge resection for small tumors (<3cm) and elderly patients
-No randomized trials, but excellent results (randomized trial 'Surgery-Radiotherapy' underway)
-Adjuvant Cisplatin-based ChT for stage II for stage IB data is conflicting
-No adjuvant radiotherapy after radical surgery (i.e. RO)
Definitive Radiotherapy for Stage I + II NSCLC
-Alternative for comorbid patients who are not fit for surgery
-For patients who refuse surgery
-60 - 66Gy to primary(+/- 50Gy to part of mediastinum, if feasible)
Review of 26 nonrandomized trials (Powell 2001)
| Cancer-specific | Survival | OS (RT) |
OS (surgery) |
| 2y | 54-93% | 22-72% |
67% |
|
3y |
22-56% | 17- 55% | |
| 5y | 13 -39% | 0-42% |
47% |
Non-cancer deaths following RT: 11 - 43%
(reflecting the poor health status of pts. treated in these studies)
-Clinical stage I only in 57% pathologic stage I (Lopez 2005)